CONTACT THE WEST GTA STROKE NETWORK REHABILITATION COORDINATOR BY PHONE AT 905-848-7580 EXT. 5683 OR BY FILLING IN THE CONTACT SHEET BELOW
Over 1/3 of stroke patients do not contact emergency medical services for transport to a hospital and only 30% of patients arriving at the hospital are getting there within the 3.5 hour time frame to be eligible for acute thrombolysis. As a result, the time to brain imaging was prolonged and the time between hospital arrival and tPA administration was over 1 hour – exceeding the target 60 minute time frame. Canadian Stroke Best Practices Recommendations added the hyperacute care guidelines with the aim to improve performance in these areas and reduce the time between stroke onset, arrival at a hospital, and treatment. The new hyperacute stroke best practices are in place to help achieve this goal and improve outcomes for all stroke patients.
Hyperacute stroke care is time sensitive and involves assessment, stabilization and treatment in the first hours after stroke or TIA onset. It represents all pre-hospital and initial emergency care for TIA and stroke. This includes thrombolysis or endovascular interventions for acute ischemic stroke, emergency neurosurgical procedures, and same-day TIA diagnostic and risk stratification evaluation.
The primary underpinnings of ‘hyperacute stroke care’ are to RECOGNIZE and MOBILIZE. This starts with recognition of stroke symptoms by patients, families, and bystanders. The Heart and Stroke Foundation has launched a new signs of stroke campaign in 2014 that uses the FAST mnemonic (FACE, ARM, SPEECH, TIME) aiming to increase recognition of the signs of stroke and take appropriate action immediately. Mobilization has to occur without delay, from emergency medical services response to a potential new stroke patient, transport to hospitals with specialized stroke services, rapid access to neuroimaging, stroke specialists and time-sensitive treatments, such as acute thrombolysis and endovascular therapy. (Canadian Best Practice Recommendations, June 2015)
A coordinated and integrated approach to hyperacute stroke care is emphasized within the West GTA Stroke Network, initiatives collaborating with Emergency Medical System, emergency departments, and other stakeholders involved in this phase of care.
INTRAVENOUS THROMBOLYSIS WITH ALTEPLASE- tPA
Background/Evidence:
What is Tissue Plasminogen Activator (tPA)?
- clot-busting drug
- must be given as soon as possible, within 4.5hrs after stroke symptoms start
- treatment with intravenous tPA can reduce the risk of death or disability following ischemic stroke at three to six-months post-treatment.
- Intravenous tPA is considered the standard of care and is currently the only approved thrombolytic agent for acute ischemic stroke treatment.
Resources:
- Canadian Stroke Best Practice Recommendations – table outlining patient selection for Acute Ischemic Stroke Treatments. Refer to box 5A and box 5C – Box-5A-5C(1)
ACUTE ENDOVASCULAR THROMBECTOMY TREATMENT-EVT
“Time is brain,” a common mantra used to describe the urgent nature of stroke care, reflects the startling reality that 1.9 million brain cells die with each minute that treatment is delayed.1 Recognizing the urgent nature of stroke, it is critical that stroke patients are identified and triaged by Emergency Medical Services (EMS) and Emergency Department (ED) hospital personnel in a timely manner.
In 2015, new evidence emerged indicating the effectiveness of endovascular thrombectomy (EVT) for the treatment of acute ischemic stroke. There have been five major trials that demonstrated efficacy with major functional benefits for patients2. The ESCAPE trail3 revealed that a procedure called Endovascular Therapy (EVT) increased positive outcomes by 25% and reduced the death rate by 50% for large ischemic strokes. New evidence from the DAWN trial has shown that in some cases hyper acute stroke treatment can now be extended up to 24 hours if the stroke patient meets the criteria.
Endovascular Treatment involves mechanical clot retrieval (embolectomy) from a large cerebral vessel performed by specialists with neuro-interventionalist expertise. It is a highly specialized procedure and performed at a limited number of sites in Ontario. Trillium Health Partners is one of the centres in Ontario that performs EVT.
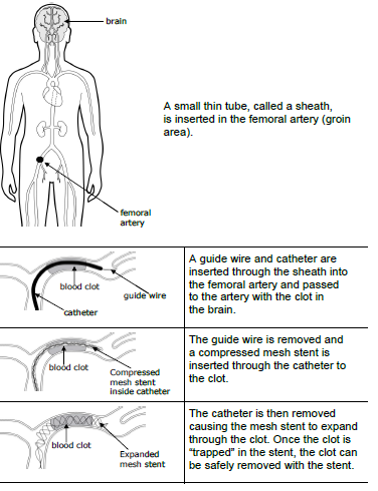
(The above image was created by the Central South Stroke Network: permission was obtained to use image Obtained from LHSC: Clot Retrieval for Stroke, Patient and Family Education pamphlet, 2017.)
Resources:
- Canadian Stroke Best Practice Recommendations – table outlining patient selection for Acute Ischemic Stroke Treatments. Refer to box 5A and box 5C – Box-5A-5C(1)
- CorHealth – Endovascular Treatment (EVT Resource Centre)
- How Endovascular Stroke Treatment works – Short youtube video
- Defining the Role of the Stroke Physician During Endovascular Therapy of Acute Ischemic Stroke – Journal Article
References:
1 Saver, J. Time is Brain – Quantified. Stroke. 2006;37:263-266. To view article CLICK HERE
2 The Mr Clean Trial was completed and demonstrated positive outcomes for patients. Subsequent to Mr Clean, the ESCAPE trial was stopped early due to overwhelming positive results and concurrent positive results of the EXTEND-IA1 trial. Two further trials SWIFT PRIME1, and REVASCAT
LARGE VESSEL OCCLUSION SCREENING TOOLS: FAST-ED and ACT-FAST
In order to efficiently triage the acute “walk-in stroke” patients presenting to our community hospitals within 12 hours, the West GTA Stroke Network (WGTASN) is introducing two LVO screening tools (FAST-ED and ACT-FAST) that will be utilized within the region. See below for more details on each LVO screening tool.
*Please be sure to refer to your specific organizations acute stroke protocols for more detail.
FAST-ED (this triage tool will be used in the region at the non-telestroke sites)
- The FAST-ED which is part of the JoinTriage App is one tool used for estimating the likelihood of large vessel occlusion. The utilization of this triage tool is to promote efficient treatment with patients presenting with acute stroke symptoms.
- FAST-ED can also be downloaded as an App called “Join Triage” on you mobile device.

- Links to FAST ED app on the Apple Store and Google Play Store
- E-Learning Education to support the use of this App:
•Please visit The WGTASN website at www.westgtastroke.ca click on the virtual classroom located on the homepage. Register yourself for the online e-learning modules and click on the FAST-ED learning module. Prior to completing the online learning download the Join Triage App to your Apple or android device. This online e-learning will take roughly 7-8 minutes to complete, the end of the module provides you with three case scenarios. You will receive a certificate of completion at the end of the module.
ACT-FAST (this triage tool will be used in the region at the telestroke sites)
- The ACT-FAST is a large vessel occlusion screen for EVT being used to guide decision making for triaging patients arriving in the Emergency Department with stroke symptoms between. The ACT-FAST algorithm has high specificity and reliability for recognizing large vessel occlusion in severe stroke.
- For more information regarding the ACT-FAST please click on the reference link.
BACKGROUND INFORMATION/WEBSITE RESOURCES
The Canadian Best Practice Recommendations (CSBPR) is intended to provide up-to-date evidence based guidelines for the prevention and management of stroke, and to promote optimal recovery and reintegration for people who have experienced stroke (patients, families and informal caregivers).
They are updated and released every 2 to 3 years with interim updates of specific topics when critical new evidence emerges.
They address the continuum of stroke care from stroke symptom onset through the hyperacute period to rehabilitation and longer-term recovery.
The target audience for the CSBPRs includes all healthcare professionals involved in the care of patients with stroke or TIA across the continuum.
Hyperacute stroke care specifically refers to the key interventions involved in the assessment, stabilization and treatment in the first hours after symptom onset. This represents all prehospital and initial emergency care for TIA, ischemic stroke, intracerebral hemorrhage (ICH), subarachnoid hemorrhage (SAH), and acute venous sinus thrombosis. This includes assessment, diagnosis with the support of early neurovascular imaging, thrombolysis or endovascular interventions for acute ischemic stroke, emergency neurosurgical procedures, and same-day TIA risk stratification and diagnostic evaluation.
Stroke Best Practices Website:
HYPER ACUTE BEST PRACTICE 2018 UPDATES
Hyper-Acute Best Practice Update: 2018 update to guidelines for healthcare providers caring for people with current or recent symptoms of acute stroke or TIA
Canadian Stroke Best Practice Recommendations: CSBPR2018 ACUTE Stroke Best Practice updates 17Jul2018 EN
BACKGROUND/INFO
Hyperacute stroke is a medical emergency and optimizing out-of-hospital care improves patient outcomes. Emergency medical services play a critical role in out-of-hospital (prehospital) assessment and management of suspected stroke patients. Acute interventions such as thrombolytic therapy are time-sensitive and therefore strategies such as re-directing ambulances to stroke centres to facilitate earlier assessment, diagnosis, and treatment may result in better outcomes.
Patients who show signs and symptoms of hyperacute stroke in the community must be treated as time-sensitive emergency cases and should be transported without delay to the closest institution that
provides emergency stroke care. Immediate contact with emergency medical services is strongly recommended because it improves the time to treatment for acute stroke.
Emergency Medical Service (EMS) dispatchers must triage patients showing signs of hyperacute stroke as a priority dispatch. EMS providers should use a standardized diagnostic screening tool. In Ontario, a Paramedic Prompt Card has been implemented for this purpose. The prompt card assists EMS providers in initially recognizing the signs and symptoms of stroke and subsequently in determining the most appropriate hospital to transport the patient.
RESOURCES
- Paramedic Prompt Card:
- Time-is-brain in acute stroke treatment and prolonged times to accessing thrombolysis and/or EVT may reduce benefits for eligible patients.
- The Paramedic Prompt Card for Acute Stroke Protocol ensures that stroke patients receive the appropriate diagnostic imaging, expertise, and treatment in a timely manner
- As of March, 2018 the time window for transport to a Designated Stroke Centre will be expanded from 4.5 hours to 6.0 hours from time of Last Seen Normal (LSN)
- Basic-Life-Support-Patient-Care-Standards-v32
The Canadian Stroke Best Practice Recommendations have excellent resources. Some of the PDF resources are attached below. Please refer to the section for more detailed information outlined Emergency Medical Services Management of Acute Stroke Patients.
- Standardized Acute Pre-Hospital Stroke Screening Tools
- Box 3A of the Canadian Stroke Best Practices outlines Core Information required by EMS.
TRANSIENT ISCHEMIC ATTACK (TIA)/ STROKE PREVENTION CLINIC
Transient Ischemic Attack (TIA):
- A TIA is often called a mini-stroke, but it’s really a major warning. TIA is a temporary blockage of blood flow to the brain. Since it doesn’t cause permanent damage, it’s often ignored. But this is a big mistake. TIAs may signal a full-blown stroke ahead
- Ideally, people experiencing any of the signs of an acute stroke should immediately go to an emergency department.
Regional Stroke Prevention Clinics:
- The Regional Stroke Prevention Clinic provides rapid access to specialized assessment, including diagnostic tests and risk-factor management, for those suspected of experiencing a Transient Ischemic Attack (TIA) or non-disabling stroke.
- Please refer to the Stroke Prevention section of our website for more details including referral form by clicking HERE
ORDERSETS AND STROKE PROTOCOLS
The establishment of a local stroke protocol at your organization is essential.
MORE INFORMATION TO COME
Examples of Stroke Ordersets:
- ED Premilinary Orderset
- Non tPA orderset
- Post tPA
- Post EVT
- CSBPR-Order-&-Documentation-Template-ED-evaluation-of-Acute-Stroke-&-TIA
*Please ensure that your organization’s stroke ordersets reflect stroke best practices. These best practices are often updated and when a
NEUROVASCULAR (BRAIN AND VASCULAR) IMAGING
- All patients with suspected acute stroke, presenting within
acute stroke treatment time windows, must undergo
immediate noncontrast brain CT imaging, and vascular imaging
with CTA including extracranial and intracranial arteries
to guide hyperacute care (2015 Canadian Best Practice
Recommendations for Stroke Care: Hyperacute). CT and CTA
should be done back to back.- CT – HEAD is ordered STAT in emergency department to rule out brain hemorrhage or identify other etiologies.
- CT – Angiogram (CTA) (Head and Neck) examines blood flow through the arteries in the neck and brain – dye is injected into a vein and a series of rapid-image x-rays are taken as the dye travels through.
TELESTROKE
Background:
Telestroke is an emergency telemedicine application using videoconferencing technology. Telestroke sites can provide assessment and treatment of patients experiencing acute stroke via consultation with a provincial Telestroke neurologist. The neurologist can view the patient’s CT scan electronically, “see” the patient using live video and discuss results with the patient’s physician.
Within the West GTA Stroke Network region there are currently two telestroke sites: Brampton Civic Hospital and Etobicoke General Hospital
Resources:
- Telestroke-Referral-Worksheet(1)
- Canadian Stroke Best Practice Recommendations : Telesroke Toolkit
NEUROLOGIC ASSESSMENT
Background/Info:
The use of a stroke scale in the assessment of the acute stroke patient has been established as best practice stroke care. The Canadian Stroke Best Practice Recommendations (CSBPR, update 2015) state: “A neurological examination should be conducted to determine focal neurological deficits and assess stroke severity [Evidence Level B]. A standardized stroke scale should be used, such as the National Institutes of Health Stroke Scale (NIHSS) or the Canadian Neurological Scale (CNS) (page 2)”
The NIHSS is a proven, reliable and valid tool in the assessment of the acute stroke patient and has become more common in influencing decisions for treatment options for stroke patients in the acute setting (i.e. thrombolysis therapy).
Within the West GTA Stroke Network region, hospital sites are either currently utilizing the NIH Stroke Scale or they are in the process of implementing the scale. As an aside, some Emergency departments within the region utilize a modified version and the in-patient units utilize the full version.
Training Options/Resources:
The NIHSS does not require certification to be used in practice, but education and training is required to attain and maintain competence in using the scale and interpreting the score. (CSBPR, Table 3.1)
“Healthcare professionals using the NIH Stroke Scale as a diagnostic tool on patients must show and document proper competency on the use of the tool. Before using the NIHSS it is important to ensure that all health care professionals are following the standards for training and certification program”. This can be found at www.NIHStrokeScale.org (pocket guide)
- Apex Innovations – online NIH Stroke Scale Learning Module
- Within the West GTA Stroke Network region please be sure to reach out to your educators regarding the NIH Stroke Scale and specific instructions with a keycode on how to register for the free online course.
- NIH Stroke Scale International
- Candian Stroke Best Practice – StrokeAssess and Prevention PocketGuide
- Includes, common signs and symptoms, types of stroke, Canadian Neurological Scale, NIH Stroke Scale, FAST signs
- Modified NIH Stroke Scale
- Resource from South Western Ontario Stroke Network:
CLINICAL RESOURCES – HYPERACUTE STROKE CARE
OTHER CLINICAL RESOURCES
Please note this section refers to other clinical resources that are not already embedded in specific other sections located in the hyper-acute stroke section of this website that may be useful to you. Should you be looking for something specific please ensure you go to the outlined section if not there please send an e-mail to the key contact person outlined below.
Professional Stoke Education Inventory:
- The Ontario Stroke Network (now part of CorHealth Ontario) created this online resource in collaboration with its stakeholders from across the province. The Professional Stroke Education Inventory includes education resources and implementation tools to support the healthcare providers in clinical practice.
Core Competencies for Stroke:
- Core Competencies of stroke care are the key clinical skills and knowledge required to enable a healthcare provider to practice at a level consistent with evidence-based stroke care. A framework has been created to support the healthcare provider acquire the education and skills to achieve a level of stroke clinical expertise. The framework includes learning objectives, resources/knowledge translation tools, and suggested evaluation methods.
- To access the resource click here
Stroke Quality Based Procedures Resource Center:
- Stroke was selected as one of the first Quality Based Procedure medical conditions to be implemented and the Ontario Stroke Network helped in the leading of the implementation.
- The Ontario Stroke Network worked closely with Health Quality Ontario, the Ministry of Health and Long Term Care and clinical experts to develop the Quality Based Procedures: Clinical Handbook for Stroke (Acute and Post-Acute).
- This resource center provides health system planners and clinicians with tools and resources to support implementation of Stroke Quality Based Procedures across the care continuum.
- To access the resource click here
HOT TOPICS IN HYPERACUTE STROKE CARE
STROKE FACTS AND GOVERNING BODIES
Additional Resources for information about heart disease, stroke and healthy living:
Canadian Partnership for Stroke Recovery
NEWS
PUBLICATIONS
New scientific articles and journals with research about hyper-acute stroke care and treatments
Time to Treatment With Endovascular Thrombectomy and Outcomes From Ischemic Stroke: A Meta-analysis (2016)
Endovascular Therapy for Ischemic Stroke with Perfusion-Imaging Selection (2015)
Endovascular Therapy after Intravenous t-PA versus t-PA alone for Stroke (2013)
Collateral Flow Predicts Response to Endovascular Therapy for Acute Ischemic Stroke (2011)
REPORTS/PRESENTATIONS/HANDOUTS CREATED BY THE WEST GTA STROKE NETWORK
- Check out the West GTA Stroke Network’s Community Stroke Resource book (updated Spring 2020). The Community Stroke Resource Book provides stroke survivors, caregivers and healthcare professionals with information on:
- Home support services
- Specific regional stroke programs and other community services
- Books, links and other stroke websites
- To access the community resource booklet please go to homepage and click on the following icon